Background
Pneumatic tourniquets are routinely used in major orthopedic surgeries such as total knee arthroplasty (TKA) to occlude arterial flow, control perioperative bleeding, and facilitate an unimpeded surgical field 1,2,3. Despite its common use, studies have shown prolonged tourniquet application to be associated with up to a 10% symptomatic incidence of thromboembolic events such as deep vein thrombosis and pulmonary embolism, which are major postoperative complications associated with increased morbidity and mortality.
Objectives
To evaluate hematologic [Von Willebrand factor (VWF), tissue plasminogen factor (TPA) and D-Dimer (DD)] and histopathologic effects of prolonged tourniquet application in Sprague Dawley rats (SD).
Methods
Male SD rats (n=37) weight ~325 grams were randomized to an experimental group (n=19) and control group (n=18). Under isoflurane anaesthesia, a cable zip-tie emulating a pneumatic tourniquet was applied around the hind-limb of experimental animals, immediately distal to the head of the femur, at a standardized tightness of 38 newtons using a standardized cable tie hand tool for 3-hours. Control animals remained anaesthetized for the same 3-hour period, but without tourniquet intervention. After 3-hours, the tourniquet was carefully removed on experimental animals. Then in all animals, tail vein blood samples were collected, animals were euthanized and tissue samples of distal vessels (femoral and saphenous arteries and veins) and surrounding soft tissues were extracted. All hematologic parameters were measured using respective Asserachrom antigenic kits (Diagnostic Stago), an enzyme immunoassay by ELISA method. Histologic investigation included a modified Carstairs stain for fibrin and platelets as well as routine hematoxylin-eosin (H&E) staining.
Results
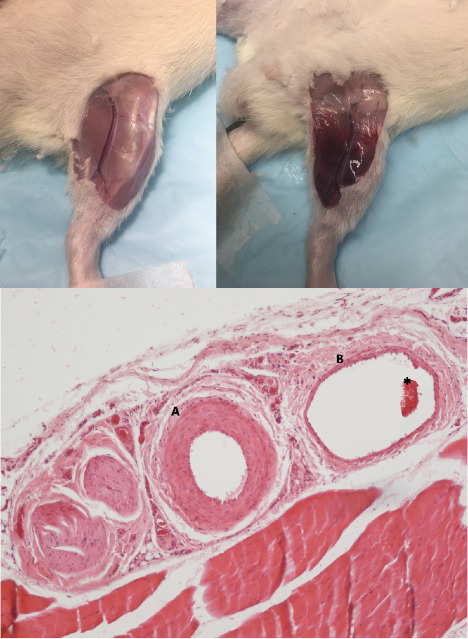
As can be seen in Figure 1, tourniquet application in the hind limb of experimental animals resulted in complete occlusion of arterial flow distal to the device, leading to bruising, muscle stiffness and bleeding into the local tissue, and associated tissue ischemia. The experimental animals exhibited elevated plasma concentration of DD (289.3 ng/mL vs 67.37 ng/mL, p<0.05), VWF (3.4% vs 2.9%, p=0.19) and TPA (11.4 ng/mL vs 1.0 ng/mL, p<0.05) when compared to its control group (Figure 1). The gross and microscopic evaluation revealed varying degrees of vascular congestion and the presence of post-mortem clot formation in the examined samples. No histological evidence of antemortem thrombosis was observed in either group in the microscopic examination of H&E slides.
Conclusion
Our animal model demonstrates prolonged tourniquet application to be associated with activation of the coagulation and fibrinolysis cascade, but did not demonstrate histological evidence of antemortem thrombosis. Future animal studies are required to compare the prevalence of thrombosis in the post-operative/tourniquet period, which would mimic the temporality of DVT development in a clinical orthopedic setting.
Figure 1:
Left: hind limb of control animal after 3 anesthetised hours of no tourniquet application. Right: hind limb of experimental animal after 3 anesthetised hours of prolonged tourniquet application. Bleeding into local tissue, and vascular and muscular tissue damage are visible. Bottom: Microscopic examination of hindlimb blood vessel. H&E staining demonstrating (A) artery, (B) vein, and (*) erythrocytes aggregation (20x magnification). There was no evidence of thrombosis.
Disclosures
No relevant conflicts of interest to declare.